What is Piles?
Piles are swollen blood vessels in the rectum and anus area. They can be internal or external and can cause discomfort, pain, and itching. Piles are a common condition that affects millions of people worldwide.
Internal piles occur inside the rectum and are usually painless, although they may cause bleeding during bowel movements. External piles, on the other hand, develop outside the anus and can be accompanied by pain, swelling, and itching.
There are several factors that can contribute to the development of piles. Some of the most common causes include straining during bowel movements, chronic constipation or diarrhea, sitting or standing for long periods, obesity, and pregnancy. Additionally, a diet low in fiber and high in processed foods can increase the risk of piles.
Piles can be categorized into four grades based on their severity. Grade 1 piles are small and may not be visible or cause any symptoms. Grade 2 piles are larger and may protrude during bowel movements but spontaneously retract afterward. Grade 3 piles also protrude during bowel movements but require manual pushing to go back in. Finally, grade 4 piles are the most severe and cannot be manually pushed back in.
What causes Piles?
Understanding the main causes of this condition can help in preventing and managing it effectively. Piles occur when the blood vessels in the anal region become swollen and inflamed. There are several factors that can contribute to the development of piles.
Poor Diet and Lifestyle
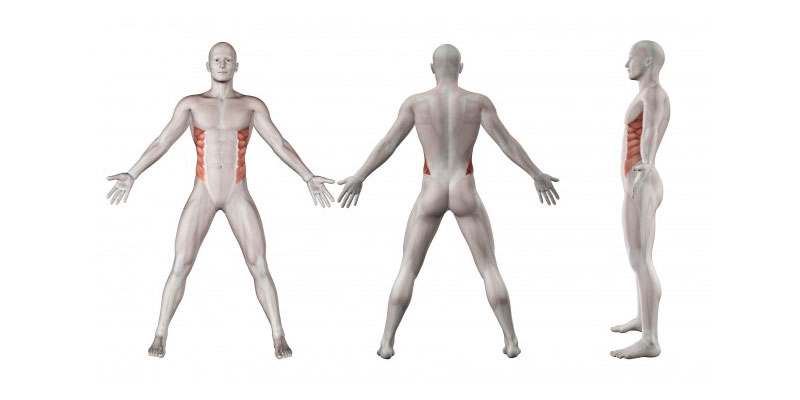
An unhealthy diet and sedentary lifestyle are common culprits behind the development of piles. A diet lacking in fiber can lead to constipation, which is a major risk factor for piles. When individuals strain during bowel movements due to constipation, it puts excessive pressure on the blood vessels in the anal area, leading to inflammation and the formation of piles. Additionally, a sedentary lifestyle with minimal physical activity can also contribute to development of piles. Lack of exercise can lead to poor blood circulation, making the blood vessels in the anal region more susceptible to swelling and inflammation.
Chronic Constipation and Diarrhea
Individuals who experience chronic constipation or diarrhea are more prone to developing piles. Chronic constipation can make bowel movements difficult and increase the strain placed on the blood vessels in the anal area. On the other hand, chronic diarrhea can irritate the anal region and cause inflammation. Both conditions can lead to the development of piles over time.
Pregnancy
Pregnancy is another common cause of piles. The growing uterus puts pressure on the pelvic veins, leading to congestion and swelling of the blood vessels in the anal area. Hormonal changes during pregnancy can also contribute to the development of piles by relaxing the walls of blood vessels, making them more prone to swelling and inflammation.
Aging
As individuals age, the connective tissues in the body tend to lose strength and elasticity. This can affect the blood vessels in the anal area, making them more susceptible to swelling and inflammation. Aging also slows down the body’s natural healing process, making it more difficult for piles to heal on their own.
What precautions you should take for Piles?
Piles, also known as hemorrhoids, are a common condition that can cause discomfort and pain. If you or someone you know is dealing with piles, it is crucial to take certain precautions to manage and prevent further complications. Firstly, maintaining good personal hygiene is essential. After each bowel movement, gently clean the area with unscented, soft toilet paper or wipes. Avoid using harsh soaps or wipes with fragrance, as these can irritate the sensitive skin around the hemorrhoids. Secondly, it is important to avoid straining during bowel movements, as this can worsen the symptoms and increase the pressure on the veins in the anal area. To do this, ensure your diet is rich in fiber and drink plenty of water to soften stools and make them easier to pass.
Furthermore, practicing proper anal hygiene can help prevent infections and reduce inflammation. Consider taking warm sitz baths for 10 to 15 minutes two to three times a day. This can provide soothing relief and promote healing. Be mindful to pat the area dry gently afterward, as rubbing can worsen symptoms. You can also apply over-the-counter hemorrhoid creams or ointments that contain ingredients like hydrocortisone or witch hazel. However, it is essential to consult with a medical professional before using any medication or cream.
In addition to taking these precautions, it is wise to avoid sitting or standing for prolonged periods of time. Sitting puts more pressure on the affected area, making the symptoms worse. If your occupation requires sitting for extended periods, try to take frequent breaks and move around to reduce the pressure. On the other hand, standing for too long can also worsen symptoms, so finding a balance is key. Engaging in regular physical activity, such as walking or swimming, can also help improve blood circulation and prevent constipation, making bowel movements easier.
If the symptoms of piles persist or worsen despite these precautions, it is crucial to seek medical advice. An accurate diagnosis and appropriate treatment plan can help alleviate the discomfort and prevent further complications. Remember, it is always better to be safe and consult with a medical professional rather than relying on self-diagnosis or self-treatment.
What are the main symptoms of Piles?
The most commonly reported symptom of piles is rectal bleeding. This occurs when the swollen blood vessels rupture, leading to bright red blood in the stool or on toilet tissue. While blood in the stool can be alarming, it is important to remember that there can be other causes for rectal bleeding as well. It is recommended to consult a medical professional for an accurate diagnosis and appropriate treatment.
Another common symptom of piles is itching around the anus. This occurs due to the irritation caused by the swollen blood vessels and their secretions. The sensation may become more intense after bowel movements and can be relieved by proper hygiene and the use of soothing creams or ointments as prescribed by a healthcare provider.
Pain, discomfort, and swelling in the rectal area are also typical symptoms of piles. These symptoms often worsen during bowel movements or when sitting for prolonged periods. The pain can range from mild to severe, and patients may experience a throbbing or pulsating sensation. Addressing these symptoms promptly is important to prevent the condition from worsening and impacting daily activities.
In some cases, piles may cause a lump to form near the anus. This lump can be sensitive to the touch and may cause additional discomfort or pain. External piles are more likely to produce these lumps, known as thrombosed hemorrhoids. A healthcare professional can assess the lump and provide appropriate management options.
How Piles is diagnosed?
Piles, also known as hemorrhoids, can be diagnosed through a combination of medical history review, physical examination, and sometimes additional tests. When you visit a healthcare professional with symptoms suggestive of piles, they will typically start by asking you about your medical history and any previous experiences with piles. This will help them understand your symptoms better and determine the possible causes.
During the physical examination, the healthcare professional will usually perform a visual inspection of the anus and rectum to check for any signs of hemorrhoids, such as swelling, inflammation, or protrusions. They may also gently perform a digital rectal examination by inserting a lubricated, gloved finger into the rectum to assess the internal hemorrhoids.
In some cases, additional tests may be necessary to confirm the diagnosis or rule out other conditions. These tests may include anoscopy, where a small tube with a light is inserted into the anus to examine the lower rectum and anal canal, or sigmoidoscopy or colonoscopy, which allow for a more detailed examination of the entire colon and rectum.
What are some of the main medical treatments for Piles?
One of the main medical treatments for piles is the use of topical creams or ointments containing corticosteroids that help reduce inflammation and itching. These can provide temporary relief and are usually applied directly to the affected area.
In more severe cases, a doctor may recommend minimally invasive procedures such as rubber band ligation, where a small rubber band is placed at the base of the hemorrhoid to cut off its blood supply, causing it to shrink and fall off. Sclerotherapy is another option, involving the injection of a chemical solution to shrink the hemorrhoid.
If the piles are large or persistently troublesome, surgical intervention might be necessary. Procedures like hemorrhoidectomy or hemorrhoidopexy can remove the hemorrhoids and provide long-term relief.
Which supplements work best with Piles?
One supplement that works well for piles is fiber. Increasing your fiber intake can help to soften stools and make them easier to pass, reducing strain on the rectal area. You can get more fiber by incorporating foods like fruits, vegetables, and whole grains into your diet. In addition to dietary fiber, you may consider taking a fiber supplement like psyllium husk or methylcellulose.
Another supplement that can be helpful for piles is probiotics. Probiotics are beneficial bacteria that can promote a healthy gut and improve digestion. Taking a probiotic supplement or consuming probiotic-rich foods like yogurt and sauerkraut can help to prevent constipation and maintain regular bowel movements. Some studies have also suggested that probiotics can help reduce inflammation in the gut and alleviate symptoms of piles.
Other supplements that may be beneficial for piles include witch hazel, horse chestnut, and Butcher's broom. These herbal supplements have anti-inflammatory properties and can help to reduce swelling and discomfort associated with piles. However, it’s important to consult with a healthcare professional before starting any new supplements, especially if you have any underlying medical conditions or are taking other medications.
Frequently Asked Question on Piles
1. What are piles?
Piles, also known as hemorrhoids, are swollen blood vessels located in the lower part of the rectum and anus. They can be either internal or external. Internal piles occur inside the rectum, whereas external piles form under the skin around the anus. Piles can vary in size and severity, causing discomfort or pain during bowel movements.
2. What causes piles?
The exact cause of piles is not known, but several factors can contribute to their development. Some common causes include chronic constipation or diarrhea, straining during bowel movements, a sedentary lifestyle, obesity, pregnancy, and a family history of piles. These factors can lead to increased pressure on the blood vessels in the rectal area, resulting in piles.
3. What are the symptoms of piles?
The symptoms of piles may vary depending on their size and severity. Common symptoms include itching, pain, and discomfort in the anal area, a lump near the anus, bleeding during bowel movements, and mucus discharge. In some cases, piles can cause anal swelling and inflammation, leading to difficulty in sitting or walking.
4. How are piles diagnosed?
If you suspect you have piles, it is essential to seek medical advice for an accurate diagnosis. A healthcare professional, such as a gastroenterologist or proctologist, can perform a physical examination of the anus and rectum. They may also conduct a digital rectal examination or use an anoscope or proctoscope to evaluate the internal structures. In some cases, additional tests like a colonoscopy or a sigmoidoscopy may be recommended to rule out other conditions.
5. Can piles be treated without surgery?
In many cases, piles can be effectively treated without the need for surgery. Lifestyle modifications and self-care measures are usually the first line of treatment. This includes increasing fiber intake to soften stools, drinking plenty of water, avoiding straining during bowel movements, and practicing good hygiene. Over-the-counter creams, ointments, or suppositories may provide relief from symptoms. In more severe cases or if conservative measures fail to provide relief, surgical options such as rubber band ligation, sclerotherapy, or hemorrhoidectomy may be considered.
6. How long does it take for piles to heal?
The healing time for piles can vary depending on the individual and the severity of the condition. In mild cases, the symptoms may improve within a few days or weeks with proper self-care measures. However, in more severe cases, it may take several weeks or even months for complete healing. It is important to follow the recommended treatment plan and consult your healthcare professional for proper guidance.
7. Can piles be prevented?
While the exact prevention of piles is not always possible, certain measures can reduce the risk of developing or worsening the condition. These include maintaining a high-fiber diet, staying hydrated, avoiding long periods of sitting or standing, practicing regular exercise, and maintaining a healthy weight. It is also crucial to avoid straining during bowel movements, as this can increase pressure on the rectal area.
8. Can piles cause complications?
Piles, if left untreated or if severe, can lead to complications. These may include the formation of a blood clot within an external pile, causing a painful condition called a thrombosed hemorrhoid. Prolonged bleeding from piles can lead to anemia (low red blood cell count). In rare cases, piles can develop into a condition called strangulated piles, where the blood supply to the pile is cut off, leading to severe pain and tissue death.
9. When should I see a doctor for piles?
It is advisable to consult a healthcare professional if you notice any symptoms of piles, such as persistent pain, bleeding, or if lifestyle modifications and over-the-counter treatments do not alleviate your symptoms. Additionally, if you experience severe pain or have difficulty passing stools, you should seek medical attention promptly as these may indicate a more serious condition.
10. Can I travel or exercise with piles?
While it is generally safe to travel or exercise with mild piles, it is essential to take certain precautions to avoid exacerbating the symptoms. If you are traveling, ensure you have access to clean toilets and take breaks to stretch and move around. When exercising, avoid high-impact activities that may increase pressure in the rectal area, and opt for low-impact exercises such as walking or swimming. Always listen to your body and stop any activity if it causes discomfort or pain.
Understand the who, what & why behind your favourite products
Brand Values | Product Philosophy | Product USPs
Read brand stories, their raison-d'etre, and understand what drives them to caringly create the highest quality products for your well-being.
Brand stories
Expert reviews you can rely upon
Expert Insights | Product Reviews | Connect with Experts
Gain valuable insights and read unbiased product reviews by subject matter Experts on Zotezo, the ultimate trust commerce platform, that empowers millions globally to make informed decisions for their wellbeing.
Expert Advisory